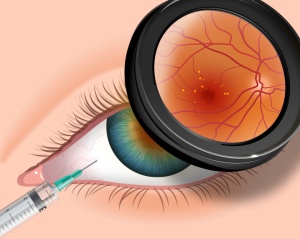
Producing milk for your newborn and perhaps even more so when you have had a very preterm infant with all the added stress is not easy. The benefits of human milk have been documented many times over for preterm infants. In a cochrane review from 2014 use of donor human milk instead of formula was associated with a reduction in necrotizing enterocolitis. More recently similar reductions have been seen in retinopathy of prematurity. Interestingly with respect to the latter it would appear that any amount of breast milk leads to a reduction in ROP. Knowing this finding we should celebrate every millilitre of milk that a mother brings to the bedside and support them when it does not flow as easily as they wish. While it would be wonderful for all mothers to supply enough for their infant and even more so that excess could be donated for those who can’t themselves we know this not to be the case. What we can do is minimize stress around the issue by informing parents that every drop counts and to celebrate it as such!
Why Is Breast Milk So Protective
Whether the outcome is necrotizing enterocolitis or ROP the common pathway is one of inflammation. Mother’s own milk contains many anti-inflammatory properties and has been demonstrated to be superior to formula in that regard by Friel and no difference exists between preterm and term versions. Aside from the anti-inflammatory protection there may be other factors at work such as constituents of milk like lactoferrin that may have a protective effect as well although a recent trial would not be supportive of this claim.
Could Mother’s Own Milk Have a Dose Response Effect in Reducing The Risk of BPD?
This is what is being proposed by a study published in early November entitled Influence of own mother’s milk on bronchopulmonary dysplasia and costs. What is special about this study and is the reason I chose to write this post is that the study is unusual in that it didn’t look at the effect of an exclusive human milk diet but rather attempted to isolate the role of mother’s own milk as it pertains to BPD. Patients in this trial were enrolled prospectively in a non randomized fashion with the key difference being the quantity of mothers own milk consumed in terms of a percentage of oral intake. Although donor breast milk existed in this unit, the patients included in this particular cohort only received mother’s own milk versus formula. All told, 254 infants were enrolled in the study. As with many studies looking at risks for BPD the usual culprits were found with male sex being a risk along with smaller and less mature babies and receipt of more fluid in the first 7 days of age. What also came up and turned out after adjusting for other risk factors to be significant as well in terms of contribution was the percentage of mother’s own milk received in the diet.
Every ↑ of 10% = reduction in risk of BPD at 36 weeks PMA by 9.5%
That is a really big effect! Now what about a reduction in costs due to milk? That was difficult to show an independent difference but consider this. Each case of BPD had an additional cost in the US health care system of $41929!
What Lesson Can be Learned Here?
Donor breast milk programs are a very important addition to the toolkit in the NICU. Minimizing the reliance on formula for our infants particularly those below 1500g has reaped many benefits as mentioned above. The availability of such sources though should not deter us from supporting the mothers of these infants in the NICU from striving to produce as much as they can for their infants. Every drop counts! A mother for example who produces only 20% of the needed volume of milk from birth to 36 weeks corrected age may reduce the risk of her baby developing BPD by almost 20%. That number is astounding in terms of effect size. What it also means is that every drop should be celebrated and every mother congratulated for producing what they can. We should encourage more production but rejoice in every 10% milestone.
What it also means in terms of cost is that the provision of lactation consultants in the NICU may be worth their weight in gold. I don’t know what someone performing such services earns in different institutions but if you could avoid two cases of BPD a year in the US I would suspect that nearly $84000 in cost savings would go a long way towards paying for such extra support.
Lastly, it is worth noting that with the NICU environment being as busy as it is sometimes the question “are you planning on breastfeeding?” may be missed. As teams we should not assume that the question was discussed on admission. We need to ask with intention whether a mother is planning on breastfeeding and take the time if the answer is “no” to discuss why it may be worth reconsidering. Results like these are worth the extra effort!





 Locally we have seen expansion of rural sites that can connect with us and a strong desire by existing sites to connect via telehealth for a variety of reasons. While the thrust of the program was to deliver advice to rural practitioners and support our level I and II units we have found such support leading to possibilities we had not dreamed of. Initial discussions via telehealth and in person have occurred examining whether such treatments as CPAP stabilization and NG feedings could be done in these sites. Being able to provide such care will no doubt lead to more stable infants being transported to our site and moreover the possibility of moving the care for infants needing only gavage feeding back to their home communities. Who knows what the future will hold for us as we also look forward to the hiring of a telehealth coordinator for NICU!
Locally we have seen expansion of rural sites that can connect with us and a strong desire by existing sites to connect via telehealth for a variety of reasons. While the thrust of the program was to deliver advice to rural practitioners and support our level I and II units we have found such support leading to possibilities we had not dreamed of. Initial discussions via telehealth and in person have occurred examining whether such treatments as CPAP stabilization and NG feedings could be done in these sites. Being able to provide such care will no doubt lead to more stable infants being transported to our site and moreover the possibility of moving the care for infants needing only gavage feeding back to their home communities. Who knows what the future will hold for us as we also look forward to the hiring of a telehealth coordinator for NICU!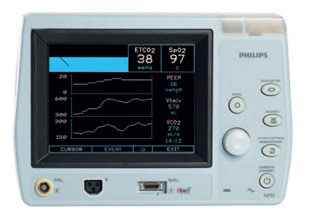 Since writing this piece we have tried it on several babies by using a double lumen tube and found the results to be as accurate as described in the Israeli papers. In practice though, secretions have proved difficult to handle for longer periods of use as they can travel up the sampling lines and damage the filters in the analyzers. A costly issue to deal with that we are currently trying to solve. Being able to continuously sample CO2 and adjust ventilation without drawing frequent blood gases is somewhat of a dream for me and we will continue to see how we can go about making this an established practice but there is work to be done!
Since writing this piece we have tried it on several babies by using a double lumen tube and found the results to be as accurate as described in the Israeli papers. In practice though, secretions have proved difficult to handle for longer periods of use as they can travel up the sampling lines and damage the filters in the analyzers. A costly issue to deal with that we are currently trying to solve. Being able to continuously sample CO2 and adjust ventilation without drawing frequent blood gases is somewhat of a dream for me and we will continue to see how we can go about making this an established practice but there is work to be done! The first is that through a generous donation and the blessing of our health region we have been able to expand the use of donor breast milk from < 1250g for a two week period to < 1500g for a one month period. This wonderful change came about after much effort and was celebrated in December as we not only expanded the eligibility criteria but partnered with the NorthernStar Mother’s Milk Bank to provide donor milk to Manitobans (
The first is that through a generous donation and the blessing of our health region we have been able to expand the use of donor breast milk from < 1250g for a two week period to < 1500g for a one month period. This wonderful change came about after much effort and was celebrated in December as we not only expanded the eligibility criteria but partnered with the NorthernStar Mother’s Milk Bank to provide donor milk to Manitobans ( The change took almost a year to roll out and could not have been done without a massive educational rollout that so many people (a special thank you to our nurse educators!) took part in. Looking back on the year we have now seen several infants at 23 weeks who survived with a small minority dying in the newborn period. It is too early to look at long term outcomes but I think many of us have been surprised with just how well many of these children have done. Moreover I believe we may be seeing a “creep effect” at work as the outcomes of infants under 29 weeks have also improved as we developed new guidelines to provide the best care possible to these vulnerable infants. Antenatal steroid use is up, IVH down and at least from January to September of last year no infants died at HSC under 29 weeks! I look forward to seeing our results in the future and cannot tell you how impressed I am with how our entire team came together to make this all happen!
The change took almost a year to roll out and could not have been done without a massive educational rollout that so many people (a special thank you to our nurse educators!) took part in. Looking back on the year we have now seen several infants at 23 weeks who survived with a small minority dying in the newborn period. It is too early to look at long term outcomes but I think many of us have been surprised with just how well many of these children have done. Moreover I believe we may be seeing a “creep effect” at work as the outcomes of infants under 29 weeks have also improved as we developed new guidelines to provide the best care possible to these vulnerable infants. Antenatal steroid use is up, IVH down and at least from January to September of last year no infants died at HSC under 29 weeks! I look forward to seeing our results in the future and cannot tell you how impressed I am with how our entire team came together to make this all happen!





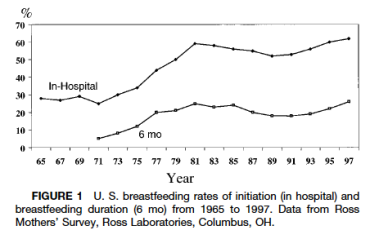
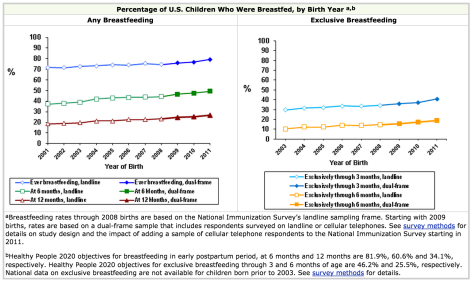
 So called Lactavists have been overjoyed to see such public acceptance and promotion of breastfeeding. As a Neonatologist I am delighted to see such high rates of breastfeeding and with it the beneficial effects that it brings.
So called Lactavists have been overjoyed to see such public acceptance and promotion of breastfeeding. As a Neonatologist I am delighted to see such high rates of breastfeeding and with it the beneficial effects that it brings.